When you open your clinic in the morning, checking schedules, reviewing last evening’s notes, catching up on lab messages, the first patient of the day reminds you how many decisions hinge on a good plan.
You’re balancing clinical detail, patient communication, insurance logistics, and the team’s workflow.
That’s why treatment-planning tools matter. They’re not just about software features; they’re about turning a busy day into one where the patient in the chair feels understood, your team feels supported, and you move through the day with fewer surprises.
Why treatment-planning tools have quickly become indispensable

In a typical practice you might juggle imaging, diagnosis, case presentation, insurance workflows and each step adds friction. Modern digital tools help reduce those friction points. They enhance diagnostics (for example with 3D imaging and software overlays) and make visualising options with patients far simpler.
Also, because patients expect clarity, speed, and collaboration, having a tool that aligns your clinical thinking with their understanding is a big win.
And yes: when you’re managing multiple patients and a growing caseload, even small workflow tweaks can mean less stress and more attention for the person in the chair.
What does effective modern-planning look like?
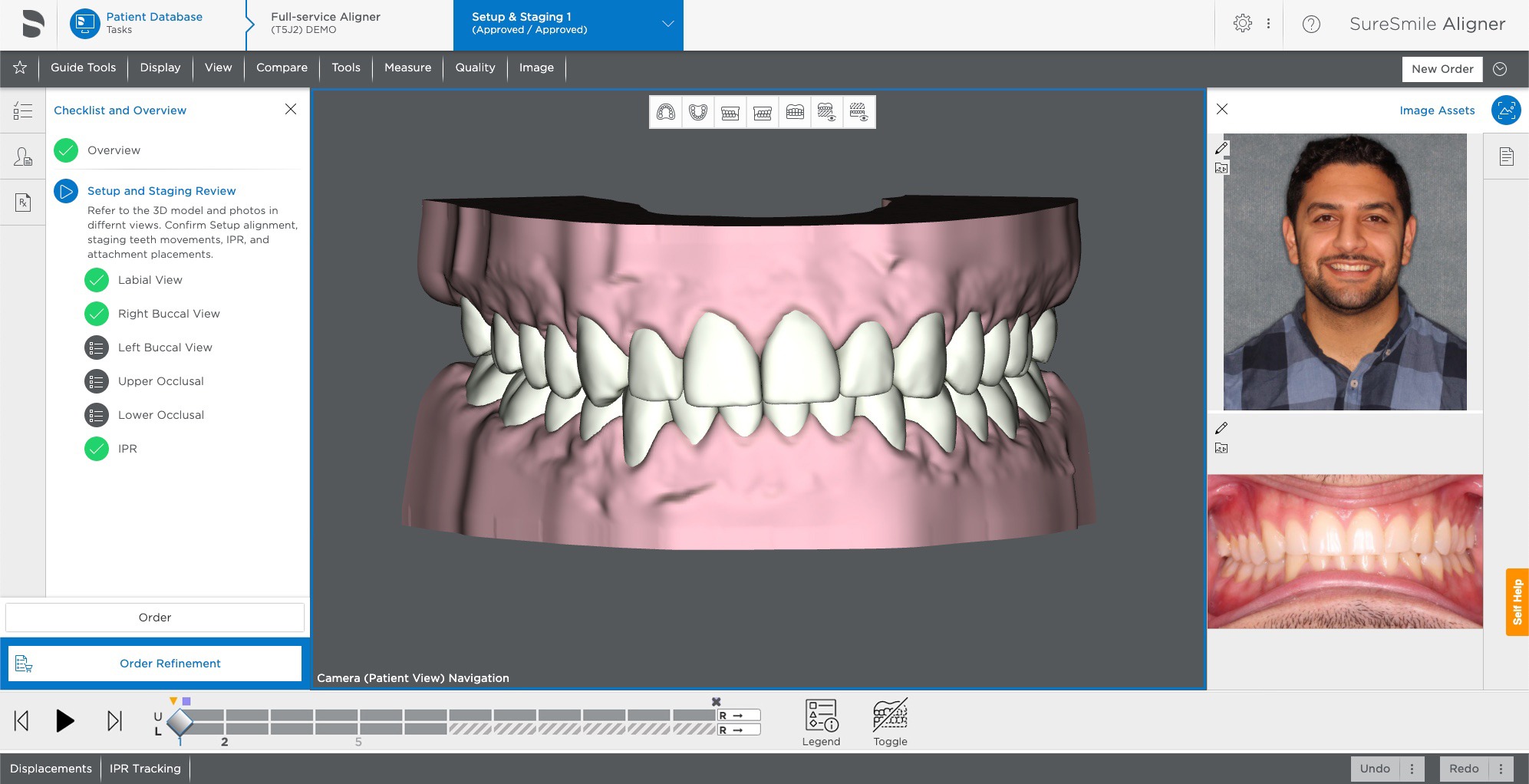
Imagine the team huddle. You open the software and you see:
- The patient’s anatomy map (digital model + imaging)
- Proposed phases (quick clean-up → restorative → follow-up)
- Budget/insurance summary visible
- Visuals you can share chairside with the patient
In more concrete terms, modern tools do things like:
- Generate treatment phases with drag-and-drop ease.
- Visualise outcomes (implant placement, prosthetic fit) with 3D views.
- Ease patient communication by turning dental codes into human language.
A note: If you’re curious which platforms deliver these features, you’ll find many options. One thing to watch for is integration, does the planning tool sync with imaging and your practice management system and the patient portal?
Did you know? Early reports suggest that practices using integrated digital planning software observe improved case acceptance through clearer patient understanding and faster chair-time.
Trust and transparency: a crucial for your patient conversations
When you present a plan, the trust your patient has in you is vital. And trust is easier to build when you share clear visuals, alternative options, and speak plain language, not only technical terms. That’s one reason the rise of AI-enhanced planning matters.
If you choose a platform that brings in advanced diagnostics without hiding it behind a black box, you’re better equipped to explain: “This tool helped highlight this interface between bone and implant and we can see why this root may respond poorly.”
If you explore tools that connect diagnosis and planning with software like Trust AI, you’re entering a space where the software supports your judgement rather than replaces it. The point isn’t “software does it all” but “software helps us do it better together.”
Key capabilities you should evaluate
Here’s a table comparing “older workflow” vs “modern-tool workflow” so you can see the impact:
| Workflow step | Older/Manual Process | With Modern Tool |
| Imaging and modelling | Manual import of CBCT/DICOM, separate software | Direct import, automatic segmentation/modelling |
| Plan creation and phases | Paper or spreadsheet, manual coordination | Drag/drop phases, visual timeline, team access |
| Patient presentation | Static printouts, verbal explanation only | 3D visuals, alternative options side by side |
| Case acceptance and workflow | Follow-up phone calls, printed worksheets | Portal links, digital signatures, clear payment maps |
| Outcome monitoring | Paper charts, post-treatment photos | Digital archive, side-by-side baseline vs outcome |
When you weigh a new tool, ask: what real time will this save? How many fewer clicks will your team make? How much clearer will the patient feel about their choice?
Real-world benefits for your clinic

- Time savings: Because imaging and planning are connected, you cut down on case prep time. One practitioner reported 30 % faster turnaround on complex cases once a planning workflow was integrated.
- Better patient engagement: Patients who see visuals of their anatomy and proposed outcome often say “okay I get it” faster—and the “do nothing” option becomes less comfortable.
- Team alignment: With one tool everyone on the team sees the same plan—hygienist, assistant, treatment coordinator—so fewer hand-offs and less miscommunication.
- Predictability: You reduce surprises during treatment because the plan is fleshed out, documented, visible, and modifiable before you start the procedure.
I’ve seen dentists light up when they realise their software can auto-populate post-treatment notes – it’s small, but it feels like a gift.
Common pitfalls (and how to avoid them)
- Over-promising technology: A tool is only helpful if you train with it and embed it into workflow. Features matter less than adoption.
- Poor integration: If the planning tool doesn’t sync with your imaging or practice-management system you’ll create parallel workflows—not save them.
- Ignoring the human side: Patients still need your explanation, empathy, and time. The tool should help—not replace—the conversation.
- Under-training your team: If assistants or coordinators don’t feel confident using the tool, it becomes a burden rather than an aid.
As you evaluate, consider asking your vendor: “What onboarding is included?” “How will we integrate it into our morning huddle, our patient presentations, the front-desk workflow?”
Where the technology is heading (and what to prepare for)
Emerging trends show increased use of artificial intelligence, augmented reality, and more seamless patient-facing visuals. For example, tools already offer:
- Automated image segmentation and diagnosis support.
- Real-time visualisation of proposed prosthetics or implant positions overlaying patient anatomy.
- Greater patient engagement via portals and interactive visual models.
As a practical preparation: ensure your clinic’s IT infrastructure (network speed, display screens, chairside monitors) is ready. Also, build a plan for how you introduce the tool to your patients in your voice, so it feels like part of your practice, not a foreign gadget.
Final thoughts
Modern treatment-planning tools are not a luxury, they’re increasingly a clinical enabler. When used well they free you to focus less on logistics and more on the person in the chair. They let you bring clarity, confidence, and collaboration into each case. From better diagnostics to stronger patient conversations, the impact is real.
Take the time to choose the right tool, train your team, align it with your daily rhythms and you’ll see that what seemed like “another software rollout” becomes instead a subtle shift: more flow, less friction, more presence for you and your patient.







